Blog Details
Diminished Ovarian Reserve (DOR)
By Dr. Sakshi Bansal / 01 January 2024Diminished Ovarian Reserve (DOR) is a condition where a woman's ovaries have a reduced quantity or quality of eggs, leading to a decline in fertility and potential difficulties in conceiving. In this article, we will delve into the causes, symptoms, diagnosis, and treatment options for Diminished Ovarian Reserve.
Diminished Ovarian Reserve (DOR) refers to a condition in which a woman's ovaries have a reduced number of eggs (oocytes) and a decline in ovarian function, which can negatively impact fertility. This condition is associated with a decrease in the quantity and sometimes the quality of a woman's remaining eggs. It is a significant factor in female infertility and can affect a woman's ability to conceive.
Age-related: DOR is often associated with advanced maternal age, typically occurring in women over the age of 35. However, it can also affect younger women.
Fertility implications: The reduced ovarian reserve can result in difficulty conceiving, a higher risk of miscarriage, and a decreased response to fertility treatments such as in vitro fertilization (IVF).
Causes: While age is a primary factor, DOR can also be caused by various factors, including genetic predisposition, certain medical treatments (such as chemotherapy or radiation therapy), pelvic surgery, or autoimmune conditions.
Diagnostic tests: Fertility specialists use several tests to assess ovarian reserve, including blood tests for hormone levels (such as Anti-Müllerian Hormone or AMH) and ultrasound examinations to evaluate the number of antral follicles in the ovaries.
Treatment options: While DOR poses challenges to fertility, there are treatment options available. Fertility treatments such as IVF may still be attempted, although success rates may be lower compared to women with a normal ovarian reserve. In some cases, assisted reproductive technologies (ART) may involve using donor eggs.
Emotional impact: Dealing with DOR can be emotionally challenging for couples trying to conceive. Seeking support from healthcare professionals, fertility specialists, and support groups can be beneficial.
Recurrent Implantation Failure (RIF)
By Dr. Sakshi Bansal / 01 January 2024Recurrent implantation failure (RIF) is a distressing experience for individuals or couples struggling to achieve a successful pregnancy through in vitro fertilization (IVF) or other assisted reproductive techniques. This condition, characterized by multiple unsuccessful embryo implantations despite several attempts, poses emotional, physical, and financial challenges. In this article, we will delve into the causes, symptoms, diagnosis, and treatment options for recurrent implantation failure.
Recurrent Implantation Failure (RIF) is a distressing condition encountered in assisted reproductive technologies, notably in vitro fertilization (IVF), where repeated attempts at embryo implantation yield persistent failures. The diagnosis is typically made after a woman undergoes several unsuccessful IVF cycles despite the transfer of high-quality embryos. RIF can be attributed to a variety of factors, including embryo quality, uterine abnormalities, immunological issues, hormonal imbalances, and thrombophilic disorders. To determine the root cause, fertility specialists employ diagnostic tests such as uterine imaging, hormonal assessments, genetic testing of embryos, and immune system evaluations. Treatment strategies for RIF vary and may involve adjustments in the IVF protocol, endometrial receptivity testing, immunotherapy, genetic testing of embryos, and interventions to address uterine abnormalities. The emotional toll of RIF is significant, impacting the well-being of couples undergoing fertility treatments. Open communication with healthcare providers and seeking emotional support are crucial components of navigating the challenges associated with recurrent implantation failure.
Pelvic Inflammatory Disease (PID)
By Dr. Sakshi Bansal / 01 January 2024Pelvic Inflammatory Disease (PID) is a serious infection that affects the female reproductive organs. It often results from sexually transmitted infections (STIs), specifically untreated or inadequately treated cases. PID can have severe consequences if left unaddressed, including chronic pelvic pain, ectopic pregnancies, and infertility. This article delves into the various aspects of PID, including its causes, symptoms, diagnosis, treatment, and implications on fertility.
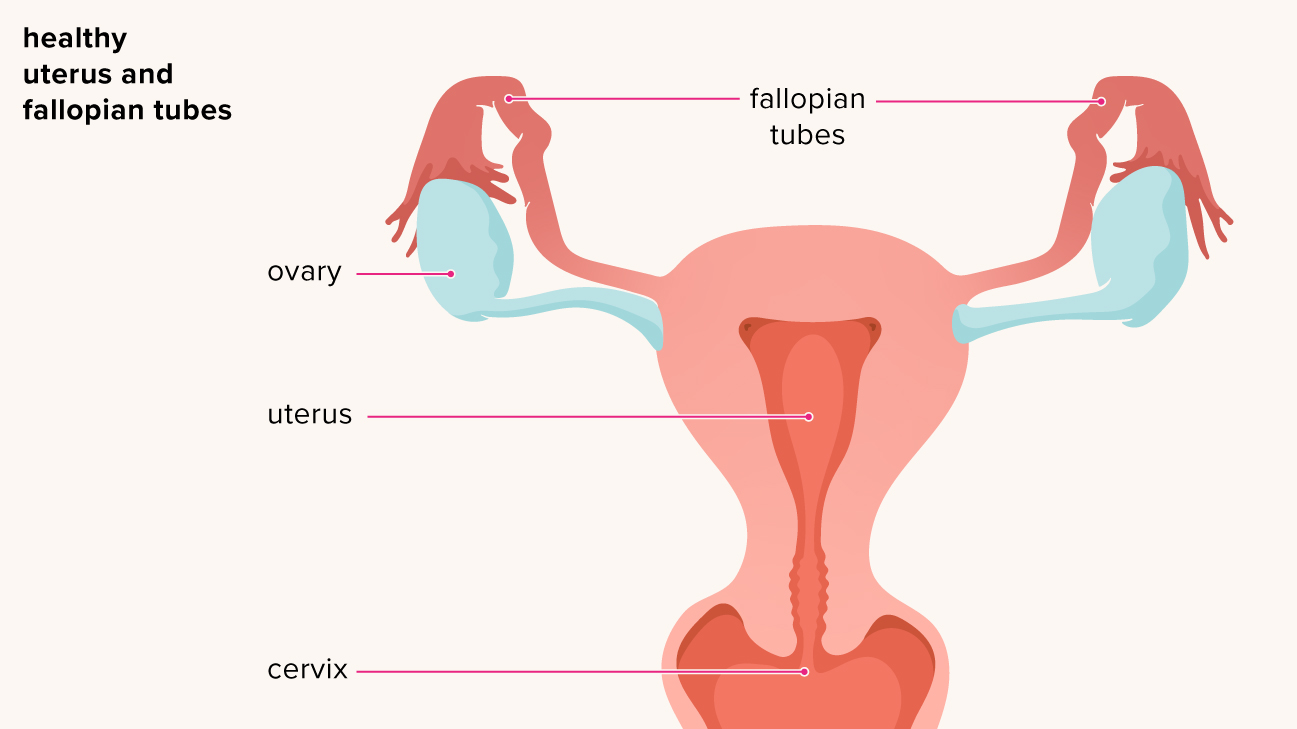
Pelvic Inflammatory Disease (PID) is a serious infection affecting the female reproductive organs, particularly the uterus, fallopian tubes, and ovaries. It typically occurs as a result of sexually transmitted infections (STIs), most commonly chlamydia and gonorrhea, but can also stem from non-STI causes such as bacterial vaginosis.
PID develops when bacteria ascend from the vagina into the upper reproductive tract, causing inflammation and potential damage.
Symptoms of PID can vary but may include pelvic pain, abnormal vaginal discharge, pain during intercourse, and fever. If left untreated, PID can lead to severe complications such as chronic pelvic pain, ectopic pregnancy, and infertility due to scarring and damage to the reproductive organs. Diagnosis involves a combination of clinical evaluation, medical history, and laboratory tests. Treatment typically includes a course of antibiotics to eradicate the infection, and in severe cases, hospitalization may be necessary.
Early detection and prompt treatment are crucial to prevent long-term complications associated with PID. Education on safe sexual practices, regular STI screenings, and open communication with healthcare providers play essential roles in preventing and managing this potentially serious condition.
 Dr. Sakshi Bansal
Dr. Sakshi Bansal